Colorectal Surgery
 Initial contact
Initial contact
A 41-year-old male patient presented at an outside hospital with pain in his pelvis and buttocks accompanied by fever and drainage from the perianal skin. He was
admitted, and a CT scan showed a large perirectal abscess with air tracking down into the left buttock and thigh with concern for a necrotizing soft tissue infection.
In the operating room, he was debrided and much of the infected and necrotic tissue was cut away. A surgeon crafted a temporary colostomy and stabilized the patient. Doctors were concerned that an underlying malignancy was behind the patient’s symptoms, and he was referred to UAMS for a consultation.
At UAMS, surgeons identified an extensive tumor in the distal rectum that had perforated the rectum and was filling most of the patient’s pelvis. It caused a fistula into the bilateral ischiorectal fossa on either side of the anus.
Assessment
During the initial surgery at UAMS, colorectal surgeons W. Conan Mustain, M.D.; Jason S. Mizell, M.D.; and their team assessed the tumor and debrided additional tissue, covering the wound with a vacuum-assisted dressing. They performed a colonoscopy through his temporary colostomy, taking biopsies that confirmed rectal adenocarcinoma. An MRI of his pelvis revealed the massive size of the tumor, which was growing into his bladder and prostate and perforating into the pelvic sidewall.
The patient needed chemotherapy and radiation before surgery would be possible. Because of increased risk for infection and other complications, chemotherapy and radiation are not typically recommended for patients with large soft tissue wounds like the patient’s, but he had limited alternatives and the medical oncology and radiation oncology teams at UAMS were willing to work with the patient and the colorectal surgery team.
The patient opted to proceed with chemotherapy and radiation in preparation for surgery.
Procedures
The patient underwent five weeks of chemotherapy and radiation with UAMS medical oncologist Rangaswamy Govindarajan, M.D., and radiation oncologist Loverd Peacock, M.D.
After the tumor shrank to an operable size, Mustain and Mizell’s colorectal surgery team joined forces with urologic oncologist Rodney Davis, M.D., and plastic surgeon Eric Jason Wright, M.D., for an 18-hour series of surgeries. The team performed a complete pelvic exenteration, removing the tumor along with the patient’s bladder, prostate, sigmoid colon, rectum, anus, distal sacrum, coccyx and other soft tissue. Mustain and Mizell established a more permanent colostomy on the patient’s left side and Davis’ team crafted a urinary stoma on the right with an ileal conduit, connecting both ureters from the kidneys to a section of small bowl.
The resection left a large empty space in the patient’s pelvis as well as a larger-than-normal soft-tissue defect on the perineum. Wright used a vertical rectus abdominis myocutaneous (VRAM) flap, taking skin and soft tissue connected to the right rectus abdominis muscle, which was flipped and rotated into the pelvis to fill the hole. The patient required additional soft-tissue to cover the presacral wound, so Wright crafted bilateral gluteal flaps from the patient’s buttocks to achieve coverage in the middle.
Follow-ups
The wound-healing time was extensive, but the patient progressed well and had a good outcome. The surgery team achieved negative margins on the cancer. At a checkup almost a year after initial contact and six months after surgery, the patient was disease free and doing well.
“This is one of the more complex cases I’ve worked on personally,” Mustain said. “With any case this complex, there are bumps in the road and unforeseen circumstances, but all told he had a great outcome. With a tumor this extensive, I think a lot of places would have recommended palliative treatment only. But we pushed and our radiation oncologists and medical oncologists were willing to give him both chemo and radiation despite his open wound, and that gave us the edge we needed.”
For a colorectal surgery referral, call 501-686-8211.
W. Conan Mustain, M.D.
Assistant professor
Department of Surgery-Colorectal
UAMS College of Medicine
Education
Medical degree, University of Mississippi School of Medicine, Jackson, Miss.
Residency
General surgery, University of Kentucky Medical Center, Lexington, Ky.
Fellowship
Surgical research fellow, Department of Surgery and Markey Cancer Center, University of Kentucky Medical Center
Colon and rectal surgery, University Hospitals-Case Medical Center, Cleveland, Ohio
Jason S. Mizell, M.D.
Associate professor
Department of Surgery-Colorectal
UAMS College of Medicine
Education
Medical degree, Louisiana State Health Sciences Center, Shreveport, La.
Residency
General surgery, Louisiana State Health Sciences Center
Fellowship
Colon and rectal surgery, Baylor University Medical Center, Dallas, Texas

The patient’s perineum at presentation, following excisional debridement. The distal sacrum is exposed and there are multiple fistulae Staging MRI shows a large tumor filling the pelvis invading the prostate (pr) and the anal sphincter (a). Sagittal view showing bladder (b), sacrum (s), and pubis (p) The patient

The patient’s perineal wound after completion of neoadjuvant chemotherapy and radiation
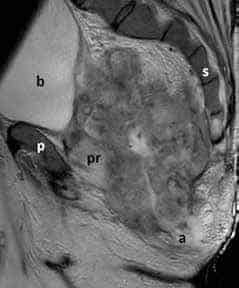
Staging MRI shows a large tumor filling the pelvis invading the prostate (pr) and the anal sphincter (a). Sagittal view showing bladder (b), sacrum (s), and pubis (p)

Following pelvic exenteration, the patient was flipped prone to debride the presacral wound and suture the VRAM flap in place.

Following pelvic exenteration, the patient was flipped prone to debride the presacral wound and suture the VRAM flap in place.

Bilateral gluteal flaps were required to achieve soft-tissue coverage over the sacral wound.