‘Pay for Performance’ Incentives Hurting Mississippi Delta Hospitals
| Oct. 30, 2017 | Two Medicare “pay for performance” programs have contributed to declining financial performance by Mississippi Delta hospitals and widening the gap in financial performance between Mississippi Delta hospitals and other hospitals in the nation, according to a study published in Medical Care by UAMS faculty.
The Hospital Readmissions Reduction Program (HRRP) and the Hospital Value-based Purchasing Program (HVBP) are having a disproportionate financial impact on Delta hospitals, according to Hsueh-Fen Chen, Ph.D., associate professor in the Department of Health Policy and Management at the Fay W. Boozman College of Public Health and lead author on the study.
The two programs provide financial incentives for hospitals to deliver higher-quality, higher-value care. The HRRP reduces Medicare reimbursements to hospitals with higher than average readmission rates for selected conditions. The HVBP adjusts payments based on a set of quality indicators.
The Delta Region is among the most socioeconomically disadvantaged areas in the United States with a high proportion of 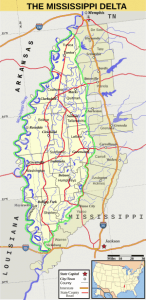 minorities. It includes 252 counties in eight states: Alabama, Arkansas, Illinois, Kentucky, Louisiana, Mississippi, Missouri and Tennessee.
minorities. It includes 252 counties in eight states: Alabama, Arkansas, Illinois, Kentucky, Louisiana, Mississippi, Missouri and Tennessee.
Chen and her colleagues compared operating margin (profitability from patient care) and total margin (profitability from patient and non-patient care) between Delta hospitals and non-Delta hospitals from 2008 to 2014 that were covered before and after implementation of the HRRP and HVBP programs in 2013.
Before implementation of HRRP and HVBP, Delta hospitals had weaker financial performance than non-Delta hospitals. Between 2008 and 2011, non-Delta hospitals had 0 percent operating margin and 2 percent to 5 percent total margin while Delta hospitals had -4 percent to -2 percent operating margin and 0 percent to 3 percent total margin.
After implementation, the gap in financial performance became significantly wider. In 2014, non-Delta hospitals had -1.5 percent and 5 percent operating and total margins, respectively. However, Delta hospitals had -10.4 percent and 0.2 percent operating and total margins, respectively. After controlling for hospital and community characteristics, the difference in operating and total margins between Delta and non-Delta hospitals remained significant.
“Delta hospitals serve as health care safety net resources and are an essential part of the health care delivery system for the people in the Mississippi Delta,” said Chen. “While the quality of care is improved nationwide, Delta hospitals are likely to get left behind and will continue to receive penalties because they have fewer resources to improve quality of care due to poor financial performance.”
This widening gap in financial performance between Delta and non-Delta hospitals under these programs is likely to widen the disparity in care between Delta and non-Delta regions.
Chen and coauthors conclude that these findings show that altering these two programs is necessary and urgent to ensure that the resources are not removed from the communities that need them most.
Her co-authors are Salema Karim, Ph.D.; Adrienne Nevola, M.P.H.; Michael Morris, Ph.D.; Mac Bird, Ph.D.; and J. Mick Tilford, Ph.D., from the Department of Health Policy and Management and Fei Wan, Ph.D., from the Department of Biostatistics.
To read the full study, go to: http://journals.lww.com/lww-medicalcare/Fulltext/2017/11000/Financial_Performance_of_Hospitals_in_the.6.aspx
